The Global Initiative for Obstructive Lung Disease, GOLD, has set out to raise clinical interest in the diagnosis and management of chronic obstructive pulmonary disease across the world [1] with the aim "to improve prevention and treatment of this lung disease". The GOLD organisation was initially a committee of respiratory specialists which was sponsored by 14 pharmaceutical companies with an interest in respiratory medical practice. It was set up in 1997 with the collaboration of the National Heart, Lung, and Blood Institute, National Institutes of Health, USA, and the World Health Organization.
The GOLD Committee arbitrarily defined COPD on clinical and physiological criteria that have been argued to be not based on scientific evidence [2]. The GOLD definition is that COPD should be considered in any patient with symptoms of cough, sputum production, or dyspnoea, and/or a history of exposure to risk factors for the disease. The diagnosis is then confirmed by spirometry showing evidence of airflow limitation. GOLD state that a post bronchodilator FEV1/FVC of < 0.7 confirms the presence of airflow limitation that is not fully reversible.
The GOLD approach has been followed in the UK by the National Institute for Health and Clinical Excellence (NICE) setting out guidelines for the management of COPD [3] indicating that any patient over the age of 35 with a risk factor for COPD and presenting with exertional breathlessness, chronic cough, regular sputum production, frequent winter bronchitis or wheeze should have the diagnosis confirmed by spirometry.
There are two reasons to question the GOLD definition of airflow limitation.
1. Using FEV1/FVC of < 0.7 to define the presence of airflow obstruction is wrong.
2. Using percent of predicted values for FEV1 to define levels of abnormality of lung function introduces age, sex and height bias.
GOLD applies a value of 0.7 for the value of FEV1/FVC to define airflow limitation. Over 50 published prediction equations for FEV1/FVC have found that this ratio falls with age [13] and so the LLN for this index also drops with age. The only publication cited by GOLD to substantiate their use of a 0.7 cut off [15] also found the ratio fell with age in women but not to a significant extent in men. This was largely because they had not adequately sampled elderly men.
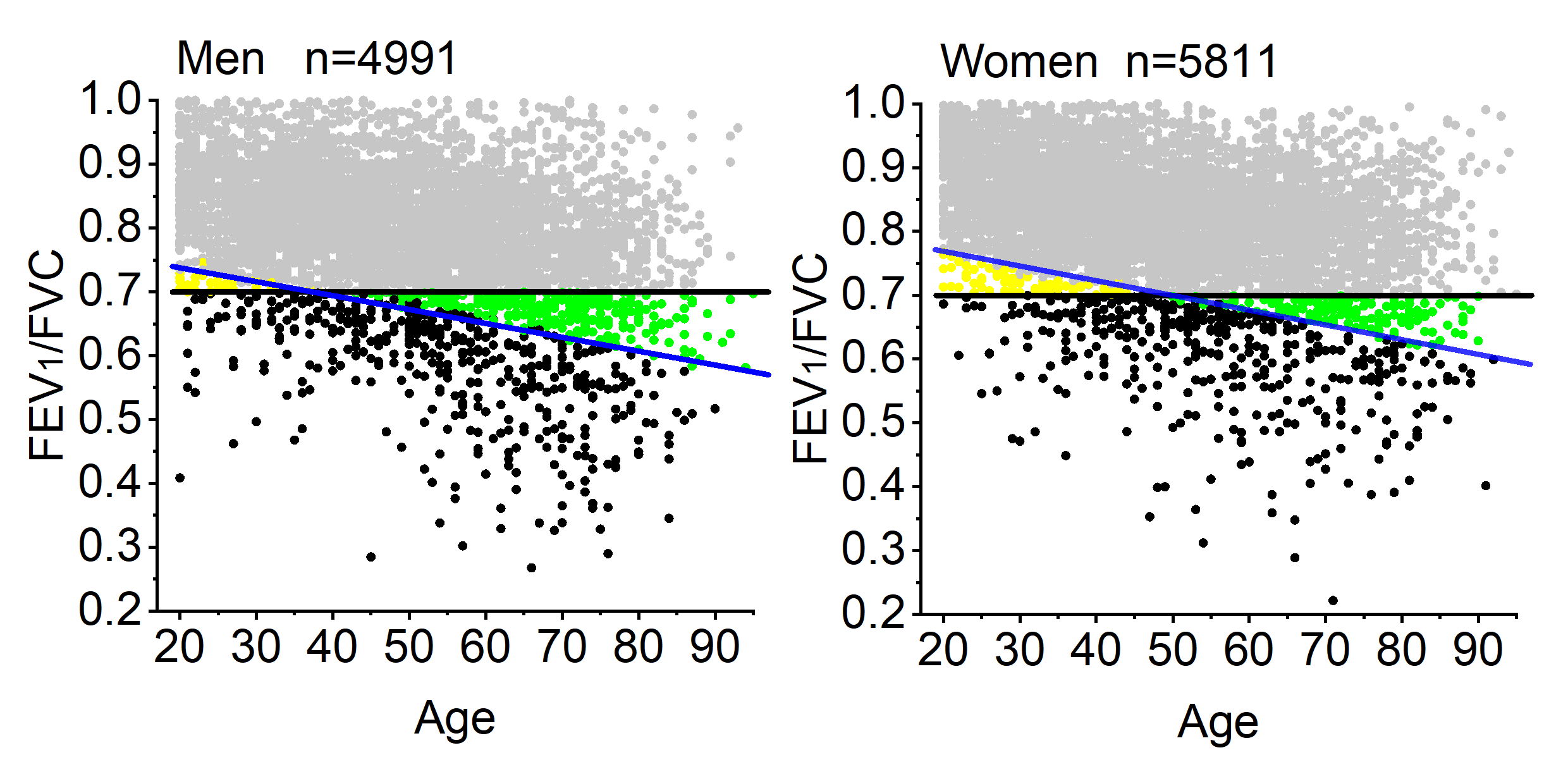
The Figure to the right shows the results for FEV1/FVC from the Health Survey of England data for 2011 [7] with men on the left and women on the right. The GOLD cut off of 0.7 is shown as a black line and the LLN from the GLI-2012 equations [14] is shown as a blue line. All the subjects plotted as pale grey dots are truly within the normal range. Those plotted in black dots are below both 0.7 and the LLN. The yellow dots are those subjects where GOLD falsely says they are normal (>0.70) but are in fact below the LLN (false negatives) and the green dots are those where GOLD says they are abnormal when in fact they are above the LLN (false positives).
When comparing the Figure for the males with that for the females it can be seen that the age at which the 0.7 cutoff changes from giving false negatives (yellow) to false positives (green) in women is about 50 yrs and is older than that found in men, approx 35 yrs.
Therefore the GOLD criterion of FEV1/FVC<0.7 for defining airflow limitation not only falsely categorises subjects but it also introduces a sex and age bias.
GOLD states that if the FEV1 is below 80% of the predicted value then this is an abnormal result.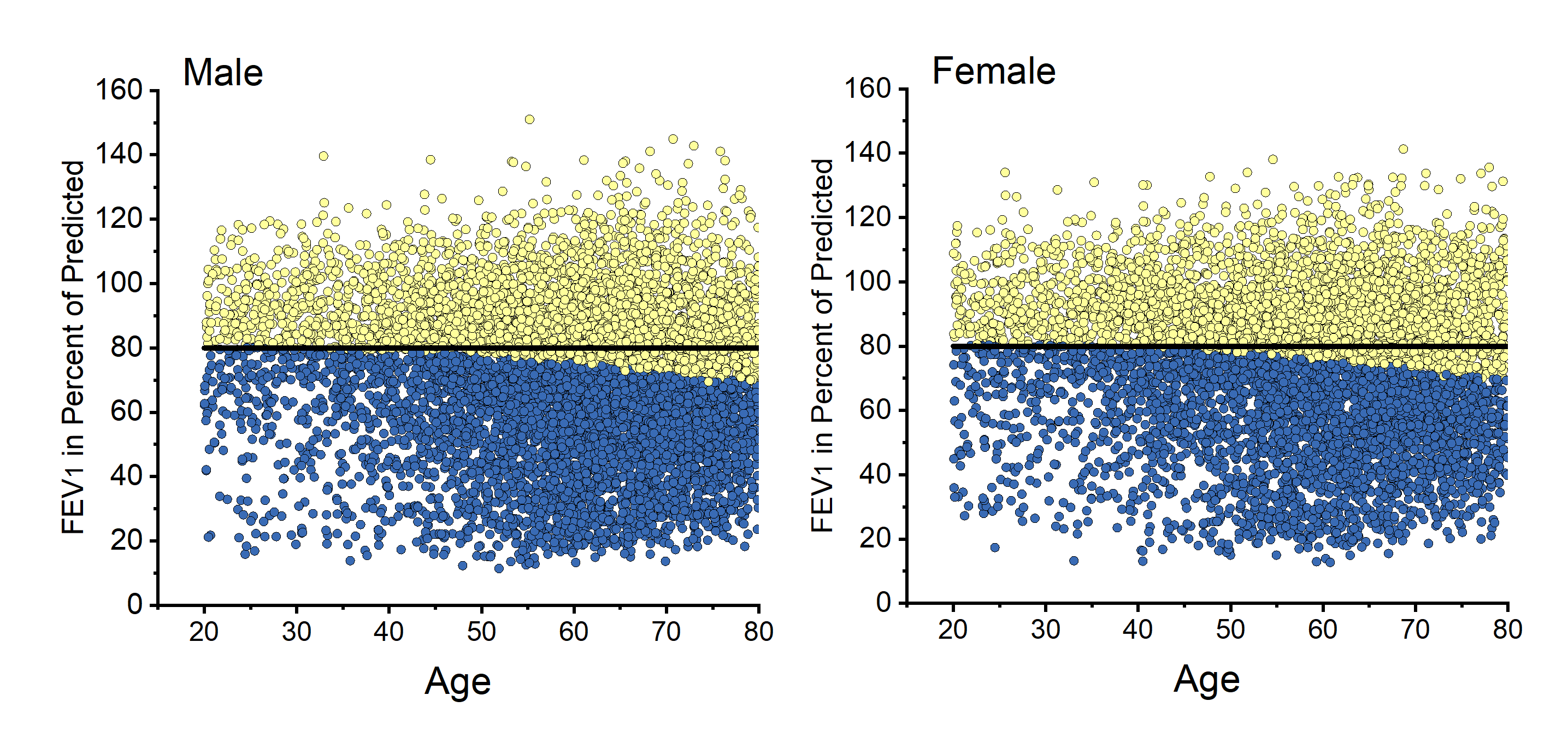 Furthermore they go on to define degrees of abnormality based on set levels of percent of predicted. FEV1 declines with age and FEV1 is larger for those of greater height. The Figure to the right shows FEV1 data for 7425 male patients on the left and 6525 female patients on the right expressed as percent of predicted (calculated from GLI-2012 equations equations [14]. Those plotted in yellow have their FEV1 above the LLN which can be seen to decline with age and those plotted in blue have their FEV1 below the LLN. The GOLD cut off of 80% of predicted as defining a normal FEV1 is evidently incorrect.
Furthermore they go on to define degrees of abnormality based on set levels of percent of predicted. FEV1 declines with age and FEV1 is larger for those of greater height. The Figure to the right shows FEV1 data for 7425 male patients on the left and 6525 female patients on the right expressed as percent of predicted (calculated from GLI-2012 equations equations [14]. Those plotted in yellow have their FEV1 above the LLN which can be seen to decline with age and those plotted in blue have their FEV1 below the LLN. The GOLD cut off of 80% of predicted as defining a normal FEV1 is evidently incorrect.
So the GOLD cut off for defining an abnormal FEV1 overestimates the number of subjects with abnormalities and this effect is greater in older subjects.
Raw FEV1 has been shown to predict future survival in patients with COPD [8] and FEV1/(ht^3) was shown in the Fletcher & Peto study to be a good way to express lung function decline in a study on COPD patients [9]. More recently FEV1/(ht^2) was found to be the best predictor of survival in the general population [10]. Stratifying lung function deficit in a cohort of COPD patients by using FEV1/(ht^2) has now been found to be better at predicting survival than both FEV1 as percent of predicted and raw FEV1 [11]. This publication showed that GOLD misclassified 50% of the patients when it came to relating their staging to subsequent survival over 15 years. Furthermore GOLD generally underestimated the severity of staging, failing to identify about one third of the subjects in the worst survival category.
New approaches to using FEV1 data have recently been published suggesting that the best signal from this lung function index with regard to survival, and presumably severity of abnormality, comes from standardising FEV1 by the cube of height or by a sex specific 1st centile value [12].
The key point here is that when considering the severity of FEV1 lung function deficit it may be better to look at how far the FEV1 is from a lower bottom line that is the survivable limit (0.5L in males and 0.4L in females) [12] rather than consider how far the value is from the subject's notional predicted value.
The GOLD criteria were set up in 1997 in an attempt to standardise the future research into COPD so that all workers in the field could work to a common standard, which is laudable. However, there was insufficient evidence at the time to substantiate their spirometric criterion for defining airways obstruction. In the light of current evidence it is clear that the GOLD criteria for tte diagnosis of COPD are flawed.
This will lead to more older subjects being diagnosed with COPD than is justified since the inclusion criteria as shown above will include a significant number of normal subjects who do not have COPD. Many of these subjects may have heart disease to account for their symptoms and will then possibly receive treatment for COPD that they do not require, which may be harmful to them [4], and bear the burden of the label of disease they do not warrant.
It is clear that the scientific community in Respiratory Medicine must act to correct this anomaly so that research into COPD is not contaminated by the rules being wrong at the start.
Copyright © 2023 Prof MR Miller - All Rights Reserved